
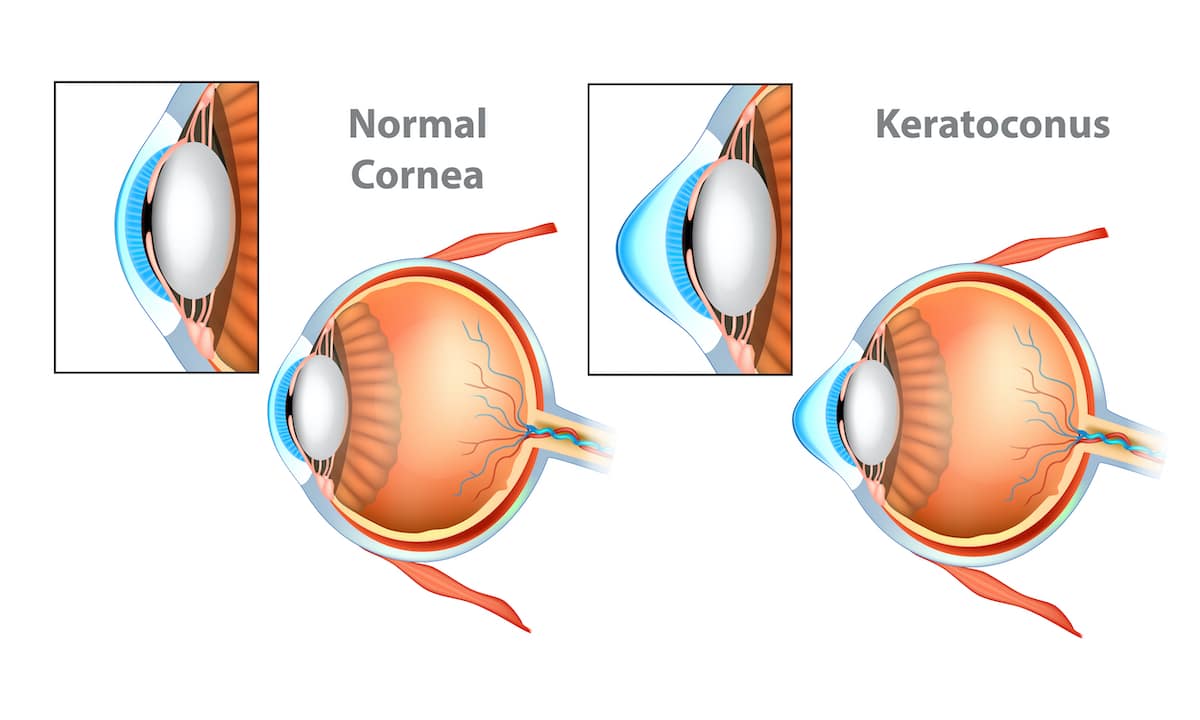
Keratoconus is an uncommon condition in which the normally round, dome-like cornea (the clear front window of the eye) becomes thin and develops a cone-like bulge. Keratoconus literally means “cone-shaped cornea.” A cornea with Keratoconus has a pointed shape more like the end of a football, rather than the side of a basketball. In most cases, a cornea with Keratoconus will be much thinner than normal. The cause of keratoconus is still not known.
Keratoconus usually affects both eyes, though symptoms in each eye may differ. Symptoms usually start to occur in people who are in their late teens and early twenties and may include:
The rate of progression varies. It will often progress slowly for 10 to 20 years and then suddenly stop. As the condition progresses, most common symptoms include:
Occasionally, keratoconus can advance rapidly, causing the cornea to become scarred. Scar tissue on the cornea causes the cornea to lose its smoothness and clarity. As a result, even more distortion and blurring of vision can occur.
The cause of keratoconus is still not known. Some researchers believe that genetics play a role since an estimated 10% of people with keratoconus also have a family member with the condition.
Treatment will often depend on the severity of the condition. During the early stages, vision can be corrected with eyeglasses. As the condition progresses, rigid contacts may need to be worn so that light entering the eye is refracted evenly and vision is not distorted. You should also refrain from rubbing your eyes, as this can aggravate the thin corneal tissue and make symptoms worse. Patients with Keratoconus are NOT candidates for refractive surgeries like LASIK and PRK. These procedures should never be done in patients with Keratoconus so as to avoid making a thin and unstable cornea thinner and more unstable.
When good vision is no longer possible with contact lenses, a corneal transplant is recommended. This surgery is only necessary for about 10-20% of patients with keratoconus. In a corneal transplant, a cornea specialist removes the diseased cornea from your eye and replaces it with a healthy donor cornea.
While a corneal transplant will relieve the symptoms of keratoconus, it may not provide you with flawless vision; eyeglasses or contacts may still be needed to achieve your best vision.